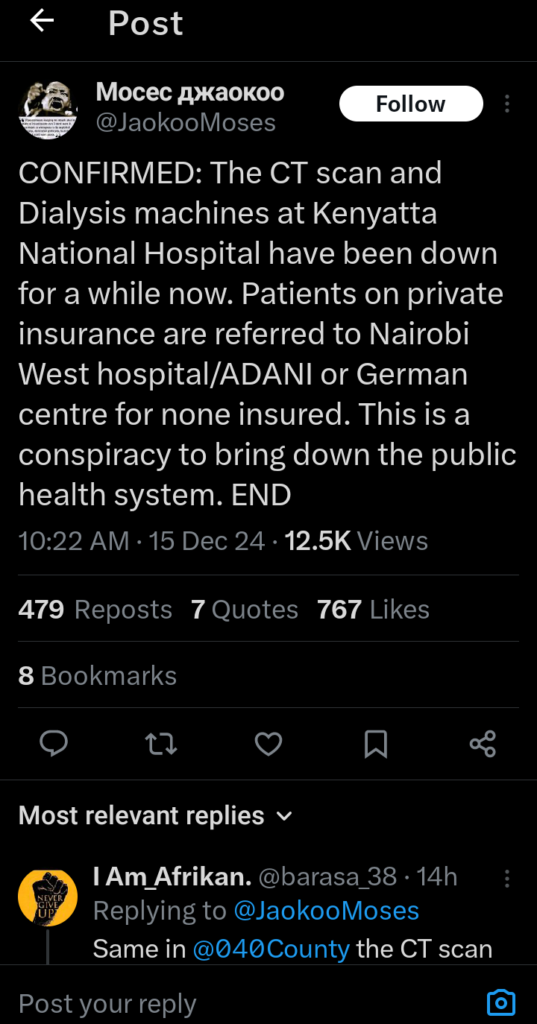
Kenyatta National Hospital (KNH), Kenya’s leading referral hospital, is grappling with a severe breakdown of essential medical equipment, including CT scan and dialysis machines.
Reports indicate that patients requiring these services are being redirected to private facilities such as Nairobi West Hospital, ADANI Medical Centre, or the German Medical Centre.
This has fueled speculation about a deliberate effort to undermine public healthcare and shift patients toward private, more expensive alternatives.
The dialysis unit at KNH, previously regarded as a lifeline for hundreds of kidney patients, is now virtually non-operational.
This development is particularly devastating considering the prevalence of kidney diseases in Kenya, which affects millions of people.
For years, KNH has been a more affordable option for dialysis, charging about KSh 5,000 per session, with NHIF subsidizing half the cost.
By contrast, private hospitals charge between KSh 7,500 and KSh 9,000 per session, making them unaffordable for many Kenyans.
The current situation has left patients with no choice but to seek costly alternatives or forego treatment altogether, with fatal consequences.
Similarly, the breakdown of CT scan equipment has disrupted vital diagnostic services.
Although KNH made strides in modernizing its imaging technology during the COVID-19 pandemic, the ongoing failures highlight a worrying lack of maintenance and operational oversight.
Patients now face delays or are compelled to seek imaging services in private hospitals, which often charge exorbitant fees.
This creates a barrier to timely diagnosis and treatment, disproportionately affecting low-income families.
The crisis at KNH reflects deeper systemic challenges in Kenya’s public healthcare sector.
Critics argue that the government’s focus on public-private partnerships and high-cost medical leasing programs has diverted resources away from adequately equipping and maintaining public hospitals.
Some allege that these failures are intentional, designed to benefit private healthcare providers while undermining public facilities.
This suspicion is reinforced by the consistent referral of patients to select private hospitals, raising questions about possible collusion between public officials and private entities.
Restoring functionality to KNH’s critical equipment should be an immediate priority for the government. Investments in regular maintenance, workforce capacity, and transparency in resource allocation are crucial to prevent further erosion of public healthcare.
Neglecting these responsibilities risks exacerbating inequalities in access to medical care and undermines public trust in Kenya’s healthcare system.
Without urgent intervention, many vulnerable Kenyans will continue to suffer, and the vision of universal health coverage will remain a distant dream.





















Add Comment